
Cedarhurst (516) 374-3668
Franklin Square (516) 775-8440

Cedarhurst (516) 374-3668
Franklin Square (516) 775-8440

Charcot foot is a rare but serious condition that can affect people with diabetes and nerve damage. It occurs when the bones in the foot weaken and begin to fracture or dislocate without causing much pain. As the condition progresses, the foot may change shape, often becoming swollen, warm, and visibly deformed. Without treatment, continued walking on the affected foot can lead to severe damage, ulcers, and even risk of limb loss. Early signs are often mistaken for a simple sprain or infection, so prompt evaluation is essential. Treatment usually involves immobilization with a cast or boot to allow the bones to heal, followed by wearing custom footwear to prevent recurrence. In advanced cases, surgery may be needed to correct deformities. If you have diabetes and notice sudden swelling, redness, or warmth in your foot, it is suggested you see a podiatrist for a diagnosis and appropriate treatment.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Robert Stein, DPM from South Shore Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Ingrown toenails develop when the edges or corners of a toenail grow into the surrounding skin, causing pain, redness, and swelling. The condition can happen on either the side, tip or even the base of the toenail. Common causes include improper nail trimming, tight shoes, or injury to the toe. In some cases, genetics or fungal infections can contribute to the development of ingrown toenails. Symptoms include localized pain, swelling, and sometimes pus or drainage if an infection sets in. The affected toe may appear red or tender, and pressure from shoes can increase the pain. Left untreated, ingrown toenails can lead to more serious complications, such as infection or permanent nail damage. A podiatrist can provide effective treatments for ingrown toenails, including trimming or removing the nail, draining any infection, and prescribing antibiotics if necessary. In chronic cases, they may perform a minor procedure to prevent the nail from growing back incorrectly. If you are dealing with an ingrown toenail, it is suggested that you make an appointment with a podiatrist for care.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Robert Stein, DPM of South Shore Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Wearing high heels for extended periods of time can lead to foot swelling due to the unnatural position they force on the feet. High heels shift body weight forward onto the balls of the feet, placing excessive pressure on the forefoot and toes. This uneven distribution of weight can restrict blood flow and cause fluid to accumulate in the lower extremities. The lack of proper arch support and narrow toe boxes in many high heels can also compress nerves and blood vessels, further contributing to swelling and discomfort. Over time, this pressure can lead to inflammation, pain, and even more serious foot conditions. Choosing footwear with better support, cushioning, and a lower heel can help reduce swelling and protect long-term foot health while still allowing for stylish options. If you have foot pain from wearing high heels, it is suggested that you contact a podiatrist who can treat various foot conditions, and guide you on appropriate heel selections.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact Robert Stein, DPM from South Shore Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
What Kinds of Foot Problems Can Develop from Wearing High Heels?
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Heel pain is a common issue that can be caused by numerous conditions like plantar fasciitis, Achilles tendonitis, or bursitis. Arthritis and gout can also play a role. Plantar fasciitis causes sharp pain in the bottom of the heel, especially with the first steps in the morning. Achilles tendonitis results in pain and swelling in the back of the heel due to overuse or strain on the Achilles tendon. Bursitis involves inflammation of the fluid-filled sacs around the heel, causing pain and swelling. Arthritis and gout can lead to joint pain, swelling, and redness, often in the heel area. The causes of heel pain vary but often involve repetitive stress, poor footwear, obesity, or underlying health conditions like arthritis or gout. The pain can range from mild to severe and can significantly impact mobility. A podiatrist can diagnose the underlying cause of heel pain and recommend treatment, such as targeted exercises, orthotics, medication, or, in severe cases, surgery. If you are dealing with heel pain, it is suggested that you make an appointment with a podiatrist.
Many people suffer from bouts of heel pain. For more information, contact Robert Stein, DPM of South Shore Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Proper toenail care is important for seniors to help prevent foot problems and maintain mobility. As people age, it often becomes harder to reach or see their feet, making basic foot care more difficult. Toenails can become thick, brittle, or discolored, and may be harder to trim. If nails are not cut properly, they can cause painful issues like ingrown toenails or infections. Seniors with diabetes or poor circulation need to be especially careful, as small problems can quickly become serious. It is important to trim toenails straight across and avoid cutting them too short. Keeping feet clean and dry also helps prevent fungal infections. If you are an older person or taking care of one and toenail care is difficult or painful, it is suggested that you visit a podiatrist who can provide professional nail trimming and check for other foot issues.
If you need your feet checked, contact Robert Stein, DPM of South Shore Foot Care. Our doctor will attend to all of your foot and ankle needs and provide you with quality treatment.
Geriatrics and Podiatry
When people age, some common issues that may occur are bone density loss, dry skin, poor circulation, and rough brittle nails. These issues may also affect your foot health if the necessary steps are not taken to alleviate the problems.
It is important to take care of your feet because feet that are injured or diseased can affect your overall health. Having painful feet hinders your ability to do daily activities or may decrease your willingness to do the things that you need to do.
Visiting Your Geriatrician
As we age, health problems become more likely, so it is essential to visit your doctor for check-ups to ensure that you are doing the best you can to take care of your health. It is recommended to check your feet frequently for any possible cuts, bruises, swelling, corns or any other irregularities.
Taking Care of Elderly Feet
Cracked or dry feet can be treated by applying moisturizer often. It is also important not to wear old socks because the older the sock is, the higher the possibility there will be that there is bacteria there. Wear fresh socks and make sure they fit properly.
Proper foot health means that you can have a more active lifestyle and you will not be bogged down by pain. Foot health also leads to good circulation, which is paramount for overall health.
If you have any questions, please feel free to contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
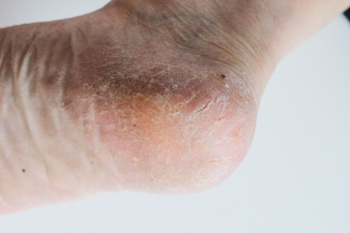
Cracked heels and fissures can develop from prolonged dryness, excessive pressure, and underlying health conditions. When the skin on the heels loses moisture and elasticity, deep cracks may form, making walking painful and increasing the risk of infection. Standing for long periods, wearing unsupportive footwear, and exposure to harsh environments can worsen the condition. Certain medical conditions like diabetes, thyroid disorders, and poor circulation can slow healing and lead to complications. If the cracks become deep, bleed, or show signs of infection, such as redness, swelling, or drainage, medical attention is necessary. Seeking care from a podiatrist early can prevent further damage and promote healing for healthier, more comfortable feet. If you have developed cracked heels, it is suggested that you consult a podiatrist who can provide appropriate treatment, including debridement, prescription creams, and specialized footwear recommendations.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Robert Stein, DPM from South Shore Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
Ways to Prevent Cracked Heels
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Foot neuropathy, often linked to conditions like peripheral artery disease, PAD, or deep vein thrombosis, DVT, can cause significant discomfort and complications. PAD occurs when blood flow to the lower limbs is reduced, leading to pain, cramping, or numbness, especially while walking. DVT, on the other hand, involves blood clots in the veins, causing swelling, warmth, and redness, which can affect mobility. Both conditions can lead to nerve damage, resulting in sensations like tingling, burning, or a pins and needles feeling in the feet. The primary causes of these issues include poor circulation, diabetes, and prolonged immobility. A podiatrist can help by diagnosing the root cause through detailed evaluations and diagnostic tests. Treatment options may include medication to improve circulation, targeted exercises, custom orthotics, or lifestyle changes. In more severe cases, surgery may be necessary. If you have foot neuropathy, it is suggested that you schedule an appointment with a podiatrist for proper care and relief.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Robert Stein, DPM from South Shore Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Gout is a rare condition in children and teenagers that occurs when uric acid builds up in the bloodstream and forms crystals in the joints. This leads to sudden, intense pain and inflammation, commonly in the big toe but also in other joints like the knees or ankles. The primary causes of gout in young people are genetic factors that cause the body to produce too much uric acid or fail to eliminate it properly. Other contributing factors may include obesity, kidney problems, or a diet high in purines found in foods such as red meat and seafood. Symptoms of gout in children and teenagers include severe joint pain, swelling, redness, and warmth around the affected area. If untreated, gout can lead to recurring attacks and long-term joint damage. If your child has symptoms of gout, it is suggested that you consult a podiatrist who can effectively treat this condition.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Robert Stein, DPM from South Shore Foot Care. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
Risk Factors
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Cedarhurst and Franklin Square, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Every patient is unique and so are treatments. The information on this website is for educational purposes and each individual
patient care model may differ.